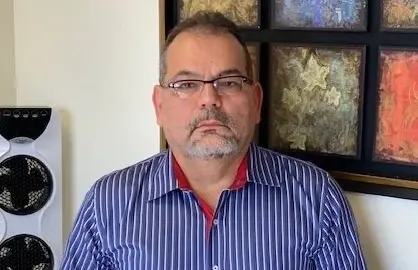
Dr. Enrique Vega joined the Global Ageing Network in March for a roundtable discussion on aging and long-term care policy in Latin America and the Caribbean. Vega, who serves as the Unit Chief for Healthy Life Course at the Pan American Health Organization (PAHO), is a medical doctor with a specialty in geriatrics. He has a long and illustrious career in public health, geriatrics, and academia including a teaching position at the Medical University of Havana since 1992.
PAHO, which was started in 1901, is the precursor to the World Health Organization. Under PAHO’s leadership, a Convention for Human Rights for Older Persons was drafted and endorsed by 11 countries, well ahead of the rest of the world which continues to debate such a convention at the United Nations. Following the tenets of the UN Decade for Healthy Ageing, Vega led the effort to draft a regional policy for long-term care which he hopes will be approved in September 2024. The focus is multisectoral, as long-term care is part of the life course. Because 90% of long-term care in the region is currently provided by women, he emphasized that the policies must support women’s lives and livelihoods. While there is no clear substitution for family care—practically or culturally—it is critical that family care be supported through social protection measures as well as increasing the capacity for paid care.
Vega spoke about workforce challenges. Less than 10% of health sciences and medical schools include any curriculum on geriatrics. And the region faces a huge challenge as a result of a “brain drain” with significant numbers of people who provide care in the region—direct caregivers, nurses, and doctors—leaving the region for better wages. As a result, a significant element of the proposed long-term care policy is focused on protecting the human resources they do have in the region and training more professionals.
The proposed framework, “Development, strengthening and scaling up long-term care in the Americas,” concludes that “the economic and social value of care should be recognized, both for those who need long-term care and for those who deliver it (paid or unpaid). People with long-term care needs and their unpaid caregivers should be actively involved in the planning, delivery, and assessment of care, considering their views and experiences as catalysts through which long-term care can be built upon and systematically improved over time.”